MRI exam with contrast – what to expect
What is it?
When is contrast necessary?
MRI contrast is given to look for inflammation, infection, cancer, blood vessel abnormality and bone marrow disorders.
In most cases, the decision to give contrast is by the clinician, depending on the clinical presentation and probable diagnosis. However, in a few cases, contrast administration has to be decided by the radiologist on-site if the “before” contrast images show an abnormality that needs further interrogation (like the case aforementioned).
How much contrast is given?
Is it safe?
A few concerns have been raised over the past few years regarding safety of gadolinium-based contrast agents (GBCAs), particularly its deposition in the brain. Scientific evidence has shown that gadolinium accumulates in brain tissues following multiple administrations. However, no adverse clinical consequences have been identified and the long-term significance of gadolinium deposition at present remains unknown. We probably won’t even know, especially if we are only dealing with a dose or two in someone’s lifetime.
The Health Sciences Authority (HSA) Singapore in one of their May 2018 publications, along with an advisory issued by College of Radiologists Singapore in 2017, stated at that point in time that there is no definitive evidence of brain diseases linked to GBCAs. Additionally, GBCAs had a long history of use with clear benefits to patients without major long-term side effects.
Side effects or reactions from GBCAs for example allergy-like reactions are uncommon, but can occur.
It is about weighing the risk benefits when making a decision to administer contrast. The thought process is, if we don’t use contrast, we may miss important clinical information on the scan, for example a cancer. So, while there may be a risk associated with administration of gadolinium, there is also a risk if you don’t administer the gadolinium when patients need it.
Contraindication to contrast
All patients who go for MRI are screened for underlying kidney problems. This is important when and if the patient requires contrast as there has been a link between GBCAs and nephrogenic systemic fibrosis (NSF) in patients with severely poor kidney function.
NSF is a rare disease where there is skin thickening and tightening and internal organ damage. About 4% of patients with severe kidney problems will develop NSF after exposure to gadolinium, a relatively small percentage.
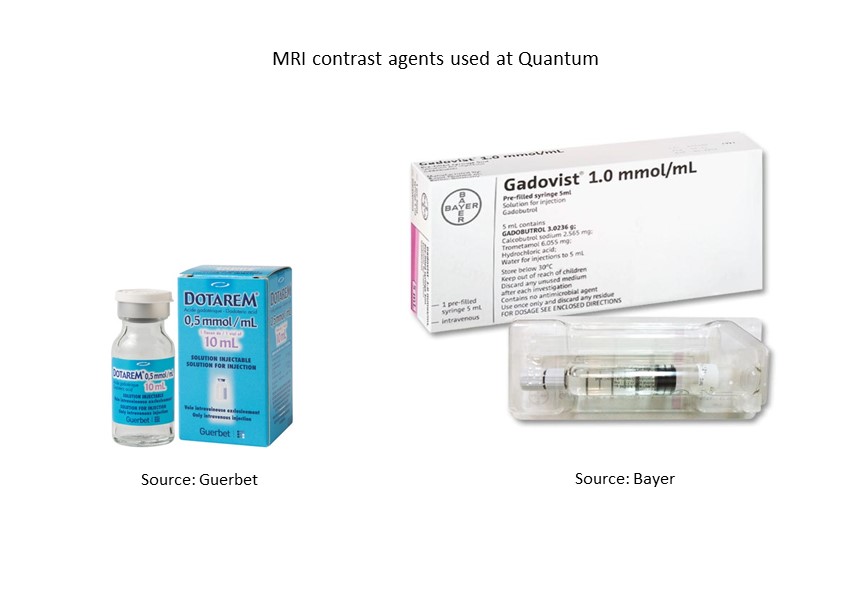
There is a form of GBCAs which seem to be of lower risk for NSF which can be used in patients with less severe kidney problems. Examples of these GBCAs are Dotarem and Gadovist/ Gadavist. This group of contrast agents have shown good safety profile not only in terms of NSF (no cases documented so far with use of these GBCAs), but also brain deposition.
References
Adverse Drug Reaction News. Published by the Health Products Regulation Group, HSA and the HSA Product Vigilance Advisory Committee ISSN: 0219 – 2152 May 2018 Vol.20 No.1.
Guo CJ, Yang ZL and Zhang LJ. Gadolinium Deposition in Brain: Current Scientific Evidence and Future Perspectives. Front Mol Neurosci. 2018; 11: 335.
Kaewlai R and Abujudeh H. Nephrogenic Systemic Fibrosis. American Journal of Roentgenology. 2012;199: W17-W23. 10.2214/AJR.11.8144.





