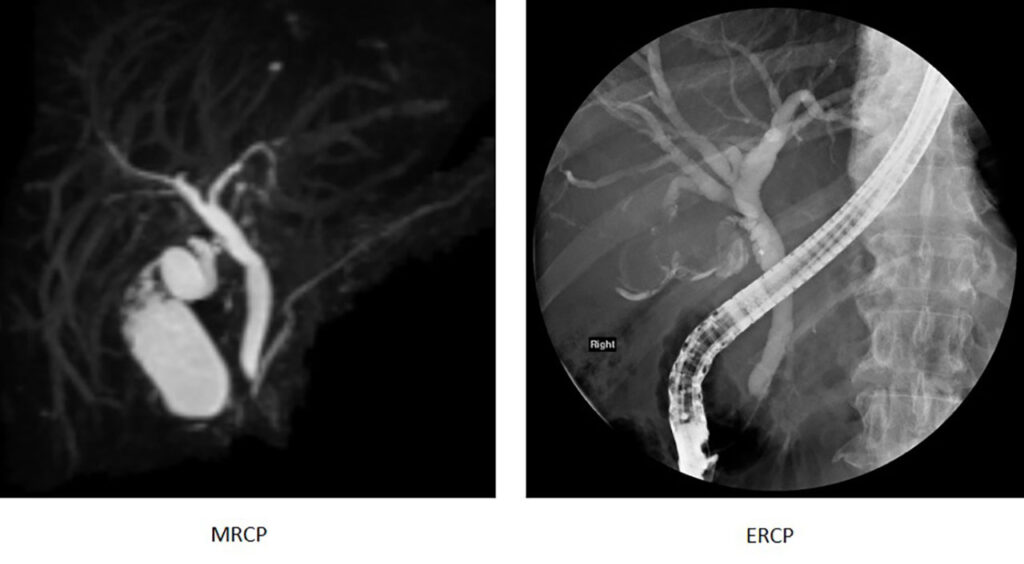
The fine-art of imaging the pancreato-biliary tree
The advent of MRCP
Clinical Indications of MRCP
MRCP is indicated in the diagnosis of many benign (non-cancerous) and malignant (cancerous) conditions that affect the bile ducts and pancreas. It is commonly used look for the following conditions:-
Biliary tree
- Check for anatomical variants of the biliary tree before surgery
- Choledochal cyst
- Bile duct stone
- Benign (non-cancerous) bile duct narrowing from inflammation
- Malignant (cancerous) bile duct narrowing from bile duct cancer (cholangiocarcinoma)

Gallbladder
- Gallbladder disease such as gallstones
Pancreas
- Annular pancreas
- Pancreas divisum
- Intraductal papillary mucinous neoplasms (IPMNs)
- Pancreatic cancer
Technique
The high water content in bile composition and its relative stasis in the bile ducts are unique properties that are exploited to aid visualisation in MRCP imaging. Thin-slices of the bile ducts as well as multiple imaging planes are obtained over 30-40 minutes. These images will then be analysed and reported by a radiologist, alongside the patient’s clinical and surgical background.
To optimise an MRCP study, pineapple juice and black tea which contain manganese, have been used but not routinely, by nulling the bright signal in the GI tract that may obscure the biliary tree. For better visualisation of the pancreatic duct, synthetic secretin, a hormone, has been injected to produce temporary distension of the pancreatic ducts.
Most importantly, patients play a vital role in the MRCP examination since they are responsible for co-operation by holding their breath and/ or staying still during the study.





