Aneurysm
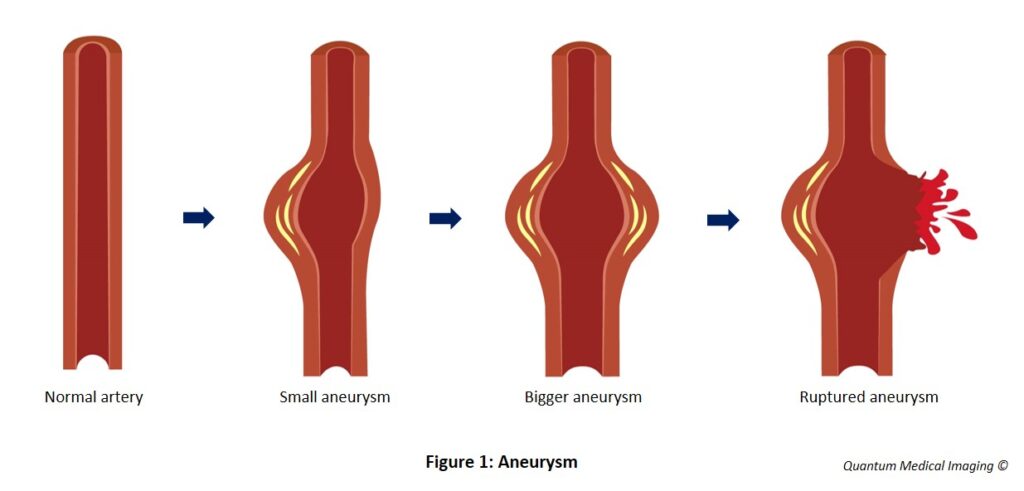
An aneurysm is ballooning of an artery. If it affects the aorta which is the body’s main artery supplying blood from the heart to all major organs, it is potentially life threatening. It is a time bomb.
Defects in part of the artery wall weaken the area, and so under pressure from blood flow, it stretches and may burst. Aneurysms can occur in any artery but the aorta is more prone to problems and the risk of death from rupture and bleeding is greatest. Abdominal aortic aneurysms are more common than thoracic aortic aneurysms.
Abdominal aortic aneurysm
Abdominal aortic aneurysm (AAA) is defined as permanent dilatation of the abdominal aorta with a diameter of 3 cm or larger. The normal diameter of an abdominal aorta is approximately 2 cm. An AAA ≥ 5 cm has a rupture risk of 1-11% per year. Most AAAs do not produce symptoms until they are detected incidentally or when they have ruptured. The risk of death from rupture is > 80%. Small AAAs can be monitored but if they grow too large i.e > 5 cm, will require a referral to vascular surgeons as they may need surgery.
Ruptured aortic aneurysm
The balloon explosion theory
Risk factors
Screening ultrasound for AAA
*Grade B indicates: A body of evidence including studies rated as 2++, directly applicable to the target population, and demonstrating overall consistency of results
Level 2++ indicates: High quality systematic reviews of case control or cohort studies. High quality case control or cohort studies with very low risk of confounding bias and a high probability that the relationship is casual.
This statement was derived from the United States Preventive Services Task Force (USPSTF) guidelines which found good evidence that screening for AAA and surgical repair of large AAA (≥ 5.5 cm or more) in men aged 65 – 75 who have ever smoked leads to decreased AAA-specific deaths. There is also good evidence that screening ultrasound is an accurate and economical screening test for AAA. Based on the moderate magnitude of net benefit, the USPSTF concluded that the benefits of screening for AAA in men aged 65-75 who have ever smoked, outweighed the harms.
Key points
- A ruptured AAA is associated with a high death rate.
- As AAA does not usually produce symptoms until late or when it has ruptured, screening should be considered in particular groups.
- Guidelines recommend that men aged 65 – 75 years old who have ever smoked may consider screening ultrasound AAA.
- Those diagnosed with a small AAA should have follow-up ultrasound for monitoring and cardiovascular risk factors modification. These patients may be referred to a cardiologist and vascular surgeon for counseling about management options.
- Those with indications for AAA repair should be referred promptly to a vascular surgeon due to impending rupture.
References
1) US Preventive Services Task Force. Screening for Abdominal Aortic Aneurysm, US Preventive Services Task Force Recommendation Statement. JAMA. 2019;322(22):2211-2218.
2) Ministry of Health Singapore, MOH Clinical Practice Guidelines 1/2011 (March 2011). Screening for Cardiovascular Disease and Risk Factors. p52.
3) Zucker EJ and Prabhakar AM. Abdominal aortic aneurysm screening: concepts and controversies. Cardiovasc Diagn Ther 2018;8(Suppl1)S108-S117.
4) Robinson D, Mees B, Verhagen H and Chuen J. Aortic aneurysms, screening, surveillance and referral. Australian Family Physician Vol 42. No. 6, June 2013.
5) Iwakoshi S, Hirai T and Kichikawa K. Updates on Ultrasonography Imaging in Abdominal Aortic Aneurysm. Annals of Vascular Diseases Vol. 12, No. 3 (2019).
6) ACR-AIUM-SRU Practice Parameter for The Performance of Diagnostic and Screening Ultrasound of the Abdominal Aorta in Adults. Revised 2020. Abdominal Aorta Ultrasound. ACR.





